As the we head into the Northern Hemisphere fall with covid-19 still raging in the US and a number of other parts of the world, two data points provide cause for extra concern.
One is that the seasonal flu–a respiratory viral infection like covid-19–is much more active in the winter. Last year in the US, there were 40 times as many flu cases in the fall and winter months as in the previous spring and summer. Historically, those cooler months see tens of times as many seasonal flu infections in temperate regions. (In tropical regions, the flu tends to peak during the rainy season, though not as strongly.)
The other is that the death toll from the 1918 influenza outbreak–the only pandemic to have killed more Americans than this one so far, and one of the deadliest in global history–was five times as high in the US during the late fall and winter as during the summer.

NATIONAL ARCHIVES
If the covid pandemic follows those patterns and blows up as we head into winter, the result could easily top 300,000 additional US deaths on top of the more than 200,000 so far, conservatively assuming (based on the 1918 outbreak) four times the rate of covid-19 deaths that we saw this summer.
How likely is that? “We just don’t have the evidence yet with this virus,” says Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota. Osterholm notes that some of the key variables defy scientific analysis and prediction. It’s difficult to calculate whether government policy will shift, whether the public will comply with guidelines, when a vaccine may become available, or how effective and well accepted it will be if it does.
Nonetheless, scientists are pulling together a picture of how the pandemic is likely to play out this winter. They are drawing on lab studies and a rapidly growing body of epidemiological data. In particular, they now better understand how lower temperatures and humidity affect the virus, and how different indoor conditions affect its transmission.
The results are not encouraging. “All the factors we associate with colder weather are looking like they will potentially accelerate the virus’s transmission,” says Richard Neher, a computational biologist at the University of Basel in Switzerland, who is developing simulations of how coronavirus spreads through a room.
The better news is that the research is also revealing steps people and institutions can take to limit transmission during the colder weather. But whether enough people will take these steps–and whether that will be enough to head off a second wave–is far from sure.
What happens to the virus in the winter?
It’s actually not typical for a new respiratory virus that becomes a pandemic to have a deadly second wave in winter. All 10 respiratory pandemics of the past 250 years had a second wave six months after the first, but in only three of those cases did it come during winter. The 1918 flu was one of those exceptions.
Could covid-19 turn out to be another? It’s hard to say. Scientists had hoped any weather-related patterns in its spread would be discernible as the months dragged on. It was early winter when the disease first broke out in China at the end of 2019, so there is now detailed data on how the virus behaves through three seasons, in both temperate and tropical climates, and through a complete summer in the Northern Hemisphere and a complete winter in the Southern Hemisphere.
No such patterns have emerged. The infection spread wildly in parts of northern Italy in March, when temperatures were already in the 70s Fahrenheit (low to mid-20s Celsius); it peaked in some US cities, such as Boston, when temperatures were in the 40s (below 10 ?C) and in others, such as Houston, when they were in the 90s (above 32 ?C). South Africa and Australia were among the Southern Hemisphere nations that saw surges during their winters, while the US was among the northern countries with summer surges. And while there’s general scientific agreement that tropical climates tend to mitigate the virus’s spread, many nations in tropical regions, including India and Brazil, have had severe outbreaks.
It would help if science had a solid, proven understanding of why the so-called seasonal flu is, well, seasonal. But it doesn’t. Linsey Marr, an environmental engineering researcher at Virginia Tech who studies viral transmission, notes that influenza viruses tend to hit hardest during the winter only after they become endemic–that is, continue to circulate year after year. That suggests seasonality may have something to do with the buildup of temporary immunity among much of the population to at least some strains of the flu. “You just don’t see that seasonality among new viruses,” she says.
Even if covid-19 turns out to show some seasonality in its first year, other factors will play a much bigger role in its spread–namely, whether people socially distance, wear masks, and avoid congregating indoors. Failure to follow these practices could explain why covid-19 infection rates skyrocketed across much of the US during the warm summer weather, when people expected it to die down. “It doesn’t mean this virus doesn’t have some sensitivity to weather,” says Benjamin Zaitchik, a Johns Hopkins University climate scientist currently studying coronavirus transmission patterns. “It may be that the effect can’t be detected against the background of policy and behavior.”
Any seasonality in covid-19 might contribute to a winter surge, however. And that could wreak havoc, because it would almost certainly coincide with the flu season. One study in the Journal of the American Medical Association found that a fifth of covid-19 patients had a second respiratory illness. Not surprisingly, they tended to be sicker on average.
An even bigger danger, says Zaitchik, is simply the combined number of covid-19 and seasonal flu cases. “It’s a health-care capacity and case management issue,” he says. “Not only will the sheer number of cases be a problem for hospitals, but doctors will have more trouble guessing which infection they’re treating when a patient first walks in.”
The good news is that the flu season in the Southern Hemisphere, May through September, was shockingly mild, almost nonexistent in many countries. The likely explanation is that masks and social distancing to protect against covid also largely prevented flu. That bodes well for the Northern Hemisphere if people continue taking those precautions.
Yet even in a mild flu year, just a small winter bump in covid-19 could have a huge impact, says Jose-Luis Jimenez, an environmental chemist at the University of Colorado. The single most important measure of whether an infectious disease can be brought under control is the so-called reproduction number, R, which indicates how many people on average will be infected by each infected person. When R is less than 1, the disease is slowing down; when it’s greater than 1, the spread is still accelerating.
If covid-19’s R is hovering at or just below 1 heading into winter, then even a small seasonal increase could push it over. “Just an extra 10% transmission during an under-control situation can blow it up out of control,” says Jimenez.
And the winter transmission boost is likely to be a lot larger than 10%, says Jimenez, because of the one factor on which virtually all experts agree: in most parts of the country people will be spending more time indoors, where the coronavirus is transmitted far more efficiently. (In the warmest parts of the country, such as Florida and Texas, it’s possible that cooler weather will encourage some people to spend less time indoors.)
A study from researchers in Japan, based on contact tracing, found that infected people were 19 times more likely to pass on the infection when they were indoors than outdoors. A database compiled by the London School of Hygiene and Tropical Medicine of about 1,500 so-called superspreader events–where a single infected person ends up infecting several other people at about the same time, in the same place–indicates that only three took place outdoors.

AP PHOTO/STEVEN SENNE
In fact, most respiratory viruses are more easily transmitted indoors. The most likely culprit is the big drop in relative humidity–the amount of water in a given volume of air compared with the maximum it could hold at that temperature–when already-dry cold outside air enters a home and is heated. The rise in indoor temperature raises the amount of water the air could hold, but the moisture level remains constant, lowering the relative humidity. A March epidemiological metastudy from researchers at Yale and in Switzerland, combined with laboratory work on mice at Yale, suggests that dry indoor air helps preserve the flu virus, and at the same time impairs the immune system’s ability to fight it off when it first takes hold in the nose or elsewhere in the airway.
Epidemiological research from MIT, Harvard, Virginia Tech, and the University of Connecticut suggests the coronavirus likewise is more infectious in low relative humidity–anything below 40% will help the virus thrive. That’s bad news for most of the US, where relative humidity routinely drops as low as 15% on the coldest days, compared with typical indoor relative humidity of 50% to 70% in the summer.
Preparations to take
One of the biggest shifts in our understanding of the coronavirus has been about how it’s transmitted. Early on, it was thought to travel in droplets of moisture from someone’s nose or mouth that would fall to the ground relatively fast. It’s now increasingly clear that tiny particles carrying the virus can remain airborne, possibly for hours, meaning they can accumulate in a room until someone breathes them in. It’s not enough to simply avoid standing too close to an infected, unmasked person indoors. People can be infected by someone who’s standing 20 or more feet away, even if they’re wearing a mask–and even if the infected person has left the room. That’s because the virus can travel farther and linger for a longer period of time, building up throughout the space.
The coronavirus does this more than most respiratory viruses–which is why many public health officials were slow to emphasize airborne transmission as covid-19’s main route of infection. Even the World Health Organization was downplaying the risk as late as July, and the Centers for Disease Control finally posted an update about airborne transmission to its website only this week, after posting and then hurriedly taking down a version last month.
Low humidity makes the risk worse, says Neher: “One of the main reasons I think we’ll see a seasonal surge in this virus is that the water in the droplets will quickly evaporate in the dry air indoors, leaving the virus in tiny nuclei that can spend more time floating around.”
Even so, many scientists doubt humidifiers will help. “To make a meaningful difference you have to add as much as five kilograms of water per hour to a room,” says Jimenez. “You’d need multiple humidifiers and you’d be refilling them often.”
GETTY
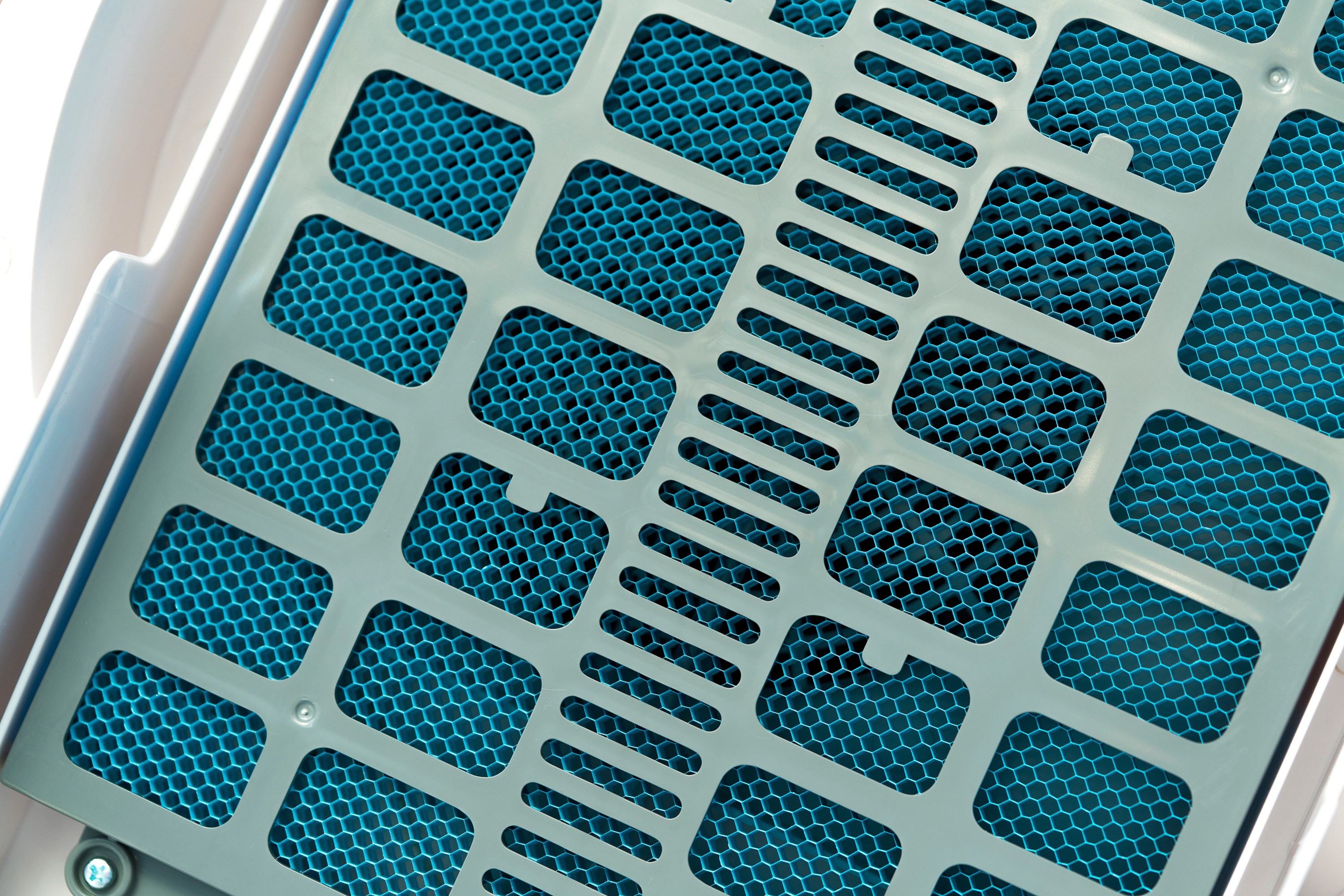
Experts say a better way to lower the risk of indoor transmission is to boost air circulation, which can disperse the plumes of virus-contaminated air from an infected person and reduce the buildup of virus in a room.
But not all air circulation is equal, warns Robert Bean, an HVAC (heating, ventilation, and air conditioning) engineer. There are several documented cases of fans or air conditioners pushing contaminated air toward people who were then infected. Moreover, the coronavirus can easily survive the ride through the heating and air-conditioning systems found in most homes.


